Why shoulder pain keeps coming back- and what you can do about it

According to a report in the Journal of Shoulder and Elbow Surgery 71% of shoulder pain sufferers are still suffering after six months. We will quickly summarise the main reasons why, then discuss these and the solution in this article.
The main reasons why shoulders don't get better
- The primary medical treatments (analgesics, NSAIDS, corticosteroids, injection therapy, surgery and physiotherapy are not evidence based (ie. they don’t work) (1,2).
- The most common diagnosis “impingement syndrome” is contradicted as a cause by scientific evidence. (3).
- Commonly prescribed exercises are shown not to help
- The two main research supported causes of shoulder pain are largely ignored by medical journals.
The good news
The good news is that the solution to a lot of shoulder problems is often to just simply do two things:
- stop doing those exercises and therapies that don’t work, and
- address the two main causes that medical journals do not tell doctors about.
CONTENTS
The medical treatments that do not work
The causes doctors are not told about
Shoulder pain treatment summary
Please note that this is for general information only. For specific advice you need a professional familiar with your own needs.
The medical treatments that do not work
In this section:
- Primary treatments
- “Impingement syndrome”
- Exercises
Primary treatments
As discussed in the following quote from the Journal of Shoulder and Elbow Surgery (1), there is no evidence the common medical treatments for shoulder pain work.
“The primary care treatment of this problem is not evidence based. Analgesia, nonsteroidal anti-inflammatory drugs (NSAIDS), corticosteroid injections, and physiotherapy modalities are all used for shoulder pain in the primary care setting. Clearly, shoulder pain is a symptom, not a diagnosis, but many studies have aimed at finding the best initial treatment for this symptom without success. Thus, trials of various interventions for shoulder pain have been performed but have been criticized for their lack of population definition and the heterogeneity of the outcome measures used.”
Impingement syndrome
Although “impingement syndrome” is the most common diagnosis made by doctors for shoulder pain, as discussed in the following quote from BMC Musculoskeletal Disorders Journal (3) this is a major error.
Although subacromial impingement is often suggested to be a potential source of shoulder pain [7,8], solid evidence is lacking. In fact, calcifications, acromion spurs, subacromial fluid, or signs of tendon degeneration are equally prevalent in healthy subjects and in patients with shoulder pain [9-12]. Furthermore, physical examination tests of subacromial impingement are not reliable [13-15], and the results of imaging diagnostics do not correlate well with pain [9,10,16,17]. In addition, interventions targeting subacromial problems are, at most, only moderately effective at treating shoulder complaints [18-24] (3).
Corrective exercises do not help
While exercises are a worthwhile part of rehabilitation, commonly prescribed “corrective exercises” do not work and can possibly make the problem worse. For more information please see our article Do exercises help shoulder pain .
The causes doctors are not told about
In the previous section we discussed that doctors are told to make incorrect diagnoses and prescribe treatment that does not work. In the following section we will discuss the two major causes of shoulder pain that:
- are supported by a large amount of research,
- treatment has been proven to be effective.
Despite being backed by a large amount of research this information is omitted from most medical journals (eg. (4,5)) This is because such information is heavily influenced by drug company funding. This affects the advice you receive, whether it is from your GP or Physio, the Mayo Clinic, or Harvard Medical School.
The causes:
Head forward posture causes shoulder pain
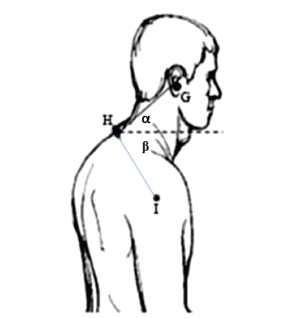
We found seven scientific studies that show that having a head and shoulder forward posture as shown in this diagram is a big cause of shoulder pain (6–12).
This causes shoulder pain by:
- affecting the balance
- affecting the mechanics of the joint

Affecting the balance
Your head and shoulders are designed to sit nicely balanced. With your head and shoulders forward they are no longer balanced, which causes extra tension on your muscles and pressure on the joints.
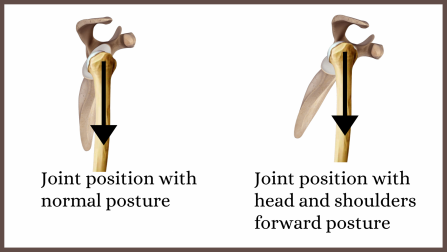
Affects joint mechanics
Having a head and shoulders forward posture changes the angle of pull on the shoulder joint and the way it moves. This can cause:
- abnormal stresses
- uneven pressure on joint surfaces
- pinching
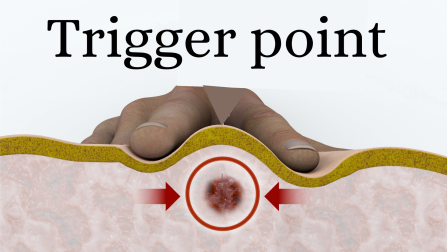
(myofascial) trigger points cause shoulder pain
(Myofascial) trigger points are those tender lumps in your muscles massage therapists find. In a series of trials, highly credentialed scientists have found that they are are a major cause of shoulder pain, and that treating them gives excellent relief (2, 3, 13–18)
These cause shoulder pain:
How trigger points directly cause shoulder pain
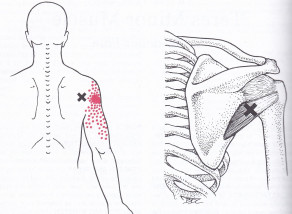
As shown in these two diagrams trigger points can refer pain to the shoulder area. Scientists have have found that trigger points in 17 different muscles are able to do this (3)
How trigger points indirectly cause shoulder pain
Shoulder function relies on muscle control
As shown in the diagram below your shoulder has a large ball sitting in a shallow socket. This allows your shoulder to move a long way, but is very unstable. Because of this your body has the muscles around the joint work as a team to keep the ball sitting correctly in place.

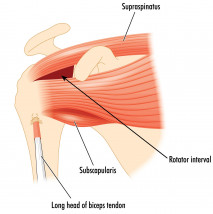
Trigger points impair muscle control
As discussed in our Your Complete Guide To (Myofascial) Trigger Points , trigger point prevent muscles from working normally. When this happens the ball does not sit in the socket correctly so:
- pressure on the bearing surfaces is uneven
- parts of the joint can be pinched or overstressed.
This can result in:
- pain
- an increased risk of injury
- increased wear (long term arthritic changes)
Shoulder pain treatment summary
Please note that this is for general information only, and no substitute for advice for advice from a professional familiar with your specific needs.
- First do no harm
- Assessment of posture
- Trigger point assessment
- Sensible use of exercises
- Medical conditions
First do no harm
The first step is to evaluate and if necessary discontinue any treatment that may be unhelpful or even harmful. For example:
- As discussed in our article Do exercises help shoulder pain , “corrective exercises” often do more harm than good.
- Analgesics may mask the pain that acts as a warning to prevent further damage.
Assessment of posture
If you have a head forward posture your shoulders will continue to suffer from abnormal stress. In one clinical trial researchers used tape to help normalise posture, however, this is not a permanent solution. There is usually a reason for this posture other than poor habits, so consciously “straightening” or doing exercises are usually not solutions either.
For more information on the common cause of poor posture please see our article on the cause of back pain. To deal with this you will likely need help from a qualified person such as a Chiropractor, Osteopath, or Physiotherapist with special post graduate qualifications.
Trigger point assessment
Please see the following article for a step by step guide on how to find and treat the trigger points that cause shoulder pain.
Massage and trigger point therapy for shoulder pain
Sensible use of exercises
So called “corrective exercises” cannot correct abnormal shoulder function are are likely to cause harm. However, once function is corrected exercises are very useful for rehabilitation. For more information please see Do exercises help shoulder pain .
Medical causes of shoulder pain
Although medical journals promote drugs and exclude other things there are some potential medical causes that can be considered. The following list is from one of the example articles that completely omitted the two major causes (4).
Potential causes of nonarthritic shoulder pain
- Rotator cuff pathology (tendonitis, tears)
- Bursitis
- Impingement
- Acromioclavicular pathology (sprains, instability)
- Labral tears
- Long-head biceps brachii pathology
- Instability
- Adhesive capsulitis/stiff shoulder
- Scapular dyskinesis
- Fracture
- Cervical radiculopathy
References
- Cloke DJ, Watson H, Purdy S, Steen IN, Williams JR. A pilot randomized, controlled trial of treatment for painful arc of the shoulder. J Shoulder Elb Surg. 2008;17(1 SUPPL.).
- Bron C, De Gast A, Dommerholt J, Stegenga B, Wensing M, Oostendorp RAB. Treatment of myofascial trigger points in patients with chronic shoulder pain: A randomized, controlled trial. BMC Med. 2011;9.
- Bron C. High prevalence of shoulder girdle muscles with myofascial trigger points in patients with shoulder pain. BMC Musculoskelet Disord 2011;12.
- Holmes RE, Barfield WR, Woolf SK. Clinical evaluation of nonarthritic shoulder pain: Diagnosis and treatment. Phys Sportsmed. 2015;43(3):262–8.
- Burbank KM, Stevenson JH, Czarnecki GR, Dorfman J. Chronic shoulder pain: Part I. Evaluation and diagnosis. Am Fam Physician. 2008;77(4):453–60.
- Jcu R, Sakthi D. Clinical assessment of subacromial impingement-which factors differ from asymptomatic population. Musculoskeltal Sci Pract. 2017;27:49–56.
- Alizadehkhaiyat O, Roebuck MM, Makki AT, Frostick SP. Postural alterations in patients with subacromial impingement syndrome. Int J Sports Phys Ther. 2017;12(7):1111–20.
- Skolimowskil J, Barczyk K, Dudek K, Skolimowska B, Demczuk-Włodarczyk E, Anwajler J. Posture in people with shoulder impingement syndrome. Ortop Traumatol Rehabil. 2007;9(5):484–48498.
- Otoshi K, Takegami M, Sekiguchi M, Onishi Y, Yamazaki S, Otani K, et al. Association between kyphosis and subacromial impingement syndrome: LOHAS study. J Shoulder Elb Surg [Internet]. 2014;23(12):e300–7. Available from: http://dx.doi.org/10.1016/j.jse.2014.04.010
- Hunter DJ, Rivett DA, McKeirnan S, Smith L, Snodgrass SJ. Relationship between Shoulder Impingement Syndrome and Thoracic Posture. Phys Ther. 2020;100(4):677–86.
- Lewis JS, Wright C, Green A. Subacromial impingement syndrome: The effect of changing posture on shoulder range of movement. J Orthop Sports Phys Ther. 2005;35(2):72–87.
- Land H. Clinical assessment of subacromial shoulder impingement – which factors differ from the asymptomatic population? Musculoskeltal Sci Pract. 2017;70:429–40.
- Gordon CM, Andrasik F, Schleip R, Birbaumer N, Rea M. Myofascial triggerpoint release (MTR) for treating chronic shoulder pain: A novel approach. J Bodyw Mov Ther. 2016;20(3):614–22.
- Sergienko S, Kalichman L. Myofascial origin of shoulder pain: A literature review. J Bodyw Mov Ther. 2015;19(1):91–101.
- Fernández-de-las-peñas AHC, Arendt-nielsen CAHGL, Arroyo-morales M. Muscle trigger points and pressure pain hyperalgesia in the shoulder muscles in patients with unilateral shoulder impingement : A blinded , controlled study . 2010;Experimental Brain Research 202(4):915-25
- Van Den Dolder PA, Roberts DL. A trial into the effectiveness of soft tissue massage in the treatment of shoulder pain. Aust J Physiother . 2003;49(3):183–8.
- Perez-Palomares S, Oliván-Blázquez B, Arnal-Burró AM, Mayoral-Del Moral O, Gaspar-Calvo E, De-La-Torre-Beldarraín ML, et al. Contributions of myofascial pain in diagnosis and treatment of shoulder pain. A randomized control trial. BMC Musculoskelet Disord. 2009;10(1):1–7.
- Hains G, Descarreaux M, Hains F. Chronic Shoulder Pain of Myofascial Origin: A Randomized Clinical Trial Using Ischemic Compression Therapy. J Manipulative Physiol Ther . 2010;33(5):362–9.
We are continually adding more information on research and uses. Subscribe below to have us email them to you "hot off the press".

About Dr Graeme
Several years ago Dr Graeme, a Chiropractor practicing in Victoria, Australia was looking for a serious hand held massager his patients could use at home to get the extra quality massage they needed. The ones he found in the shops and on-line for home use looked nice but were not serious, and... read more
