Trigger point therapy guide
(Myofascial) trigger points are an important cause of most musculoskeletal pain syndromes, plus have a host of other detrimental effects.... Read Article

Those experienced with courses of trigger point therapy such as dry needling, manual therapies and laser will understand that any relief is usually just temporary.
From an evidence perspective the problem is that while there are a large number of clinical trials supporting the use of various therapies, those trials almost universally only measure symptomatic effects, often just immediately post treatment or with a minimum follow up. The few trials that checked for the presence of trigger points post treatment all showed that most were still there, where of course they are able to continue to develop and likely be re-aggravated.
In this guide we will show you:
To understand why clinical results are misleading it is necessary to look at the typical trigger point development cycle, then what the clinical trials actually demonstrate.
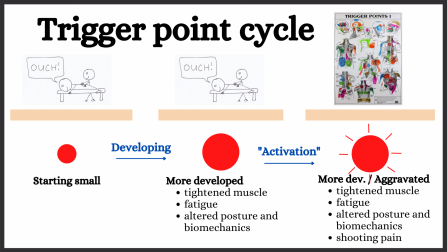
As shown in this diagram trigger points start small and gradually develop. For a long period of time they cause muscle tightness and impaired function, but are otherwise asymptomatic. When further developed though aggravation can cause them to start shooting pain. This is called “activation”.
For more info: Your Complete Guide To (Myofascial) Trigger Points
The goal of most clinical trails is to deactivate the trigger points (1–5). Deactivate simply means to revert the trigger point to how it was before it was activated, ie. to stop it shooting pain. Because of this researchers choose to only measure symptomatic and temporary factors such as:
These measurements are often made shortly after treatment, with occasional follow ups of a week or rarely a month.
We were able to find four trials that checked for the presence of trigger points post treatment (6–9). These conclusively show that even after courses of 12 extensive therapy sessions the majority of trigger points are still there, where of course they continue to develop and are eventually re-activated.
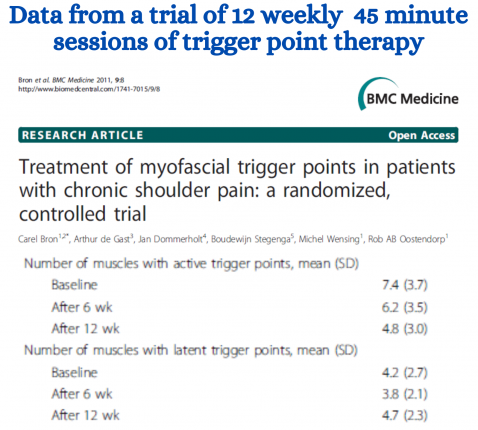
This data is taken from one trial where 12 weeks of extensive therapy with multiple therapies was given by world class trigger point researchers (7). Note that this is way more than a typical patient would receive when consulting a professional. While patients received a lot of relief approximately 2/3 of the trigger points remained.
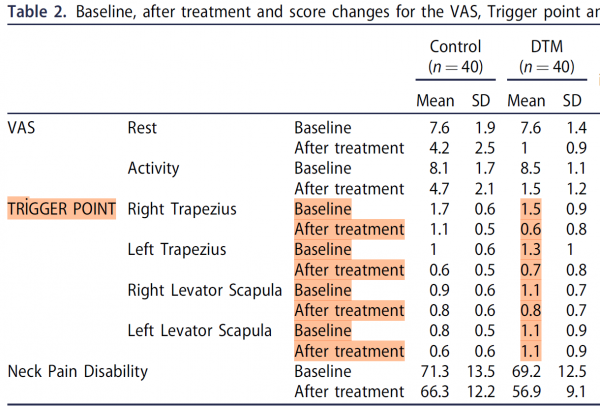
This table of data is from a trial where patients received 12 sessions of treatment including deep tissue massage, TENS and heat packs (9). Again the patients felt better, but the data clearly shows that most of the trigger points remained.

The overwhelming majority of clinical trials of trigger point therapy do the equivalent of an electrician resetting a circuit breaker and telling you they have fixed the fault. Researchers understand this.
Prior to conducting a clinical trial every researcher does an extensive literature search to find out what has already been done and what is already known. They would all have read the studies that show that their course of treatment will not eliminate the trigger points, so they deliberately choose to not check for the presence of trigger points after or measure long term effects. They then use terms such as those following to help give the appearance that their treatments are more beneficial than they actually are.
This term gives the impression that the treatment somehow makes the trigger points safe or harmless, like deactivating a bomb, whereas the reality it is just like resetting a circuit breaker.
Researchers use the term ‘acute effects” rather than than simply saying “for a short time only”.
In their conclusion researchers will say that the treatment they were testing “is effective”, but this is only in relation to the typical short term symptomatic things they measure. This is a lot different to what a clinician or patient would expect from an “effective” treatment.
Unfortunately those conducting trials on trigger point therapies have spent a massive amount of time and effort producing studies on short term symptomatic relief rather than long term elimination of the problem. To work out an effective long term strategy we need to piece together information from these and other studies relating to trigger points. Let us look at these.
While the clinical trials give no evidence about the ability to the various therapies to eliminate trigger points they do give clues about their relative effectiveness (1-4,8,15–42). As a general observation:
While the four trials that checked for the presence of trigger points after treatment found that most were still there a percentage were eliminated and the others had diminished. This indicates that further treatment will likely continue to diminish and eliminate trigger points.
Of the four trials that did check whether trigger points were still present after treatment the trial in example one above gives the best data (7). To summarise this patients received 12 weekly sessions. At each session multiple therapies were used under the supervision of world class trigger point researchers. Approximately 1/3 of the trigger points were eliminated.
It is only an indication, but at that rate 36 sessions would have been needed to eliminate all the trigger points. When considering that the sessions used in the trials were very extensive involving multiple therapies (more extensive than a typical professional visit) it likely that more than 36 typical professional visits would be needed. This would require the patient to attend a very expensive course of treatments that would extend way beyond when they felt better: something that very few would actually do. Therefore, to eliminate trigger points patients need to have a safe, easy to do effective self trigger point therapy so they can do at least some of the therapy themselves.
When assessing what is needed to effectively treat trigger points the clinical trials are not much help. They test a variety of treatments, each being roughly equal in relation to the temporary symptomatic measures tested. To work out the best treatment we need to look at the structure, pathology, physiology and neurology of trigger points to get an idea of how treatments may be effective, then chose an appropriate remedy.
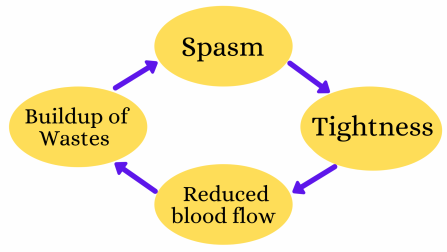
There are a large number of studies investigating the structure, pathology, physiology and neurology of trigger points. Many are extremely complex, however these can be condensed into the following summary. Trigger points are a combination of the following, forming a positive feedback loop as shown in this diagram.
The nature of positive feedback loops is the while elements remain they will continue to develop and continue to grow. The only way to eliminate trigger points completely is to completely eliminate the trigger points and address any issues that may be causing them to develop.
This model explains why there are so many different therapies shown to help. Any therapy will help if it reduces any part of the positive feedback loop. For example massage helps relax muscles, increase circulation and mechanically pump out waste products.
There are a host of potential causes and contributing factors for trigger points. We will cover these below, however the two main issues are overuse/repetitive injuries and muscle tightness. Muscle tightness may have a host of courses ranging from postural issues (eg sitting at a desk) and occupational issues (eg overuse) through to emotional stress.
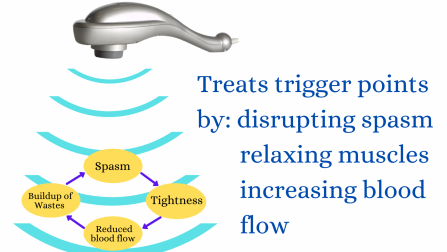
The trigger point therapy we recommend is the use of therapeutic vibration massage. We have used this extensively in clinic giving great results.
From the scientific perspective, as discussed in our guide The scientifically proven effects of vibration massage- with clinical applications therapeutic vibrations penetrate deeply and have been shown to be very effective at reducing each of the four elements of the positive feedback loop. Further, the use of vibration massage has the following advantages
Like ultrasound (vibrations at a different frequency) therapeutic vibrations can easily penetrate deeply to the hard to get at spots where a lot of trigger points are situated.
Genuine vibration massagers have a head or pad that sits on the surface and sends in vibrations, so there is little physical penetration. Therefore vibration massage is extremely safe and comfortable.
While our Vibration massage usage guide gives several precautions and ways to increase effectiveness the fundamentals are very simple. One only needs to place the head/pad of a vibration massager over the trigger point and allow the therapeutic vibrations to penetrate.
Note: this in not percussion massage (massage guns)
As shown in the diagrams below percussion massagers are designed to give physical penetration rather than send in vibrations. While they do give some vibrations those are a lot less than a genuine vibration massager and not at the optimum therapeutic frequencies. They give much reduced amounts of therapeutic vibrations while increasing the risk of physical injury or damage. In summary they are a marketing gimmick that is far less effective and less safe than a genuine vibration massager. For more info please see: Massage guns explained .

The simple strategy to eliminate trigger points is to:
Regular therapy needs to be applied for long after the symptoms subside, and until examination shows that the trigger points have been eliminated. Following that, regular (but less frequent) therapy needs to be applied to prevent further trigger points from developing.
The only practical way for most people to have this is by using at least some self therapy. The only such therapy that is safe, easy to do and highly effective is using vibration massage. All a person needs to do is sit the head/pad of a vibration massager over the trigger points and allow the vibrations to penetrate and have their therapeutic effects. For details please see our Trigger point therapy guide .
As mentioned above massage guns are designed to drive their heads in like jackhammer rather than send in vibrations so they are not suitable. The other commonly prescribed self therapy is pressure using balls or rollers. This is painful, hard to do, and confirmed by clinical trial results not very effective. For more information please see our guide Do foam rollers work . Further, because they are painful and hard to so patients are unlikely to continue with these long term if asymptomatic.
There are a number of things that to help prevent trigger points. Most involve minimising or eliminating the two main underlying causes: overuse and tightened muscles. Let’s look at some examples.
As we have seen existing trigger points cause muscles to tighten and restrict blood flow. Because of the positive feedback this cause more trigger points to develop and the existing ones to worsen. Therefore, effectively treating trigger points helps prevent further development.
Emotional tension and stress and be a significant cause of muscle knots, especially in the head and neck muscles. As an example, during the exam period in Chiropractic College fellow students sought regular treatments. This is not our area of expertise, so if this is a concern we advise that you seek appropriate advice.
Issues with your spine and posture are a very common cause of muscles to be abnormally tight. For more information about this and what to do please see this article
Causes of muscle knots can easily be minimised, but it is practically impossible top eliminate them altogether. Therefore it is great to do some ongoing muscle care to keep them from tightening and to keep an excellent blood flow. To do this we recommend:
Most of our massagers sell through colleagues using our machines and recommending the therapy to patients/clients, so we are very happy to send appropriately qualified professionals a complimentary sample machine to trial. For more info please see our Professional sample sample page .
We are continually adding more information on research and uses. Subscribe below to have us email them to you "hot off the press".

Several years ago Dr Graeme, a Chiropractor practicing in Victoria, Australia was looking for a serious hand held massager his patients could use at home to get the extra quality massage they needed. The ones he found in the shops and on-line for home use looked nice but were not serious, and... read more
(Myofascial) trigger points are an important cause of most musculoskeletal pain syndromes, plus have a host of other detrimental effects.... Read Article
Hand held massagers have allowed us to have massages without the expense and appointments needed when using a professional therapist. ... Read Article
A recent study published in the journal Asian Pacific Journal of Cancer Prevention showed that a simple 15 minute back massage each day... Read Article
Studies have shown that those suffering lower back pain have have inhibited sensory feedback and control. This lack of control is... Read Article
Foam rollers have become a popular way to have practically unlimited self massage. They are inexpensive and can easily be carried to... Read Article
Clinical trials have shown that massage is effective in relieving fibromyalgia. However, the results show that some are better than... Read Article
Most professional athletes and sports clubs make heavy use of massage type treatments. The ability to do self massage using a hand held... Read Article
Do not refresh or leave this page until loading complete.