Example two: USA's National Academy of Sports Medicine (NASM) guidelines
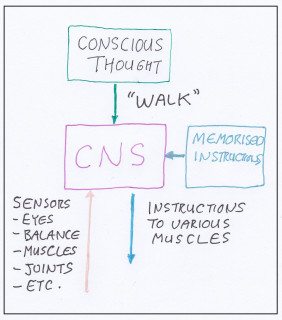
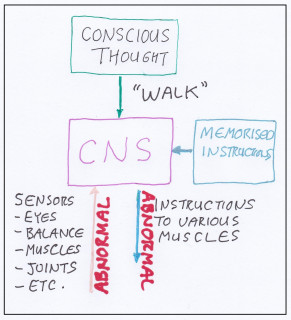
The USA’s National Academy of Sports Medicine in their publication NASM’s Essentials of Corrective Exercise Training (1) advise that to remove impediments for normal function the following procedures be included into correction exercise plans. We consider these a big improvement on the common practice of prescribing "corrective exercises" without any considerations, but it neglects to mention the very important articular considerations discussed in the next example.
- Inhibitory techniques to relax hypertonic muscles
- Lengthening techniques for contracted muscles
- Activation and integration techniques
Example three: Clinical trial
In clinical trials comparing the use of exercise alone and exerises plus manual therapies that help address muscular and articular function abnormalities, the results were far superior when the manual therapies were included (2,3). This shows the extreme importance of addressing articular functional issues. The evaluation and correction of these requires specialised knowledge and training, such as that posessed by a Chiropractor, Osteopath or a specialist Physiotheapist.