Self massage for high blood pressure
Fibromyalgia is a sensitisation of the nervous system which causes pain to be amplified plus a host of other symptoms. While there are... Read Article

According to the Mayo Clinic website the cause of fibromyalgia is said to be unknown, but thought to relate to changes in the levels of various blood chemicals and the way your nervous system processes pain messages. These changes cause symptoms such as widespread musculoskeletal pain and many others, but is there something that causes the blood chemical and nervous system changes- an underlying or root cause of fibromyalgia, and if so is it something that can be prevented or treated?
Scientists have found that there are actually many such causes, with the most common being an easily treatable source of musculoskeletal pain. They have actually treated this condition, relieving fibromyalgia, but unfortunately doctors and drug companies make a lot more money out of treating symptoms so these causes get ignored.
In this article we’ll look at how these underlying causes cause the changes in blood chemistry and neurological function that give you all those symptoms. We’ll also discuss how scientists have relieved fibromyalgia by treating these, then share with you the most common of these underlying causes and most importantly how you can treat this yourself.
Fibromyalgia: the underlying causes and effects
Why this is important for treatment
Using this information to help your fibromyalgia
What are trigger points (the most common cause)

The simplest way to describe fibromyalgia is as a sensitisation of the nervous system so it acts like an amplifier, making normal stimuli painful and pain feel much worse. Because your nervous system controls your body sensitisation can also cause those changes in blood chemical levels and seeming unrelated symptoms such as fatigue, poor sleep and digestive problems(1–7). Now let's look what causes your nervous system to become sensitised in the first place.
Sensitisation can be caused by anything that bombards your nervous system with something it cannot handle. Here are some examples.
Anything that bombards your nervous system with pain over a long period of time can cause your nervous system to become sensitised. This may be something like an arthritic joint or a back condition, but the scientists found that by far the most common cause is (myofascial) trigger points, those tender lumps in your muscles that therapists find (2,3,8,9).
This can be some form of long term stress, or sudden emotional trauma.
It is not uncommon for fibromyalgia to start after a medical condition or even after a vaccination.
When you have more than one form of stress their effects add together. Your nervous system may be able to handle the individual stresses, but when they combine they may exceed the threshold. As an example, a person may have long standing pain from one condition, then when exposed to an additional stress such as a disease or emotional trauma his or her nervous system is unable to cope. However, once the nervous system is sensitised, even if the disease or emotional trauma is removed the remaining long standing pain may prevent the nervous system from returning to normal.
The changes to the blood chemistry and the way the nervous system processes pain that the Mayo Clinic website describes are the cause of the symptoms, but are just a description of what happens when your nervous system is sensitised. In other words they are just a symptom or an effect of the underlying stress or continued bombardment of your nervous system. As we will see, doctors treat these changes as a cause rather than effects. This is the main reason the medical treatments for fibromyalgia at best only temporarily relieve symptoms.
To illustrate why understanding cause vs effects is so important we’ll:
As we mentioned the biggest cause of sensitisation is (myofascial) trigger points bombarding your nervous system with pain. This can either be on their own, or added with another form of stress. The way scientists successfully relieved fibromyalgia was to simply inject the trigger points with anaesthetic, stopping them from bombarding the nervous system with pain (10). Of course injections of anaesthetic wear off, so this is not a practical long term solution, but it proved the concept- if you take away the underlying cause of sensitisation all those effects like the blood chemicals and the way the nervous system process pain settle down.
When doctors and others think that the cause is blood chemicals and the way the nervous system processes, they look at all sorts of ways to alter the blood chemistry and suppress the nervous system. This also applies to others recommending diets and other therapies, again targeting those changes. These can never cure fibromyalgia, and mainly benefit the huge industry built around providing those symptom relieving drugs and other therapies.
The scientists found that if you remove the cause of the sensitisation the nervous system can return to normal and the symptoms settle down. There are many possible causes so this can take some detective work. What we’ll do now is share with you some very important considerations, then some specific information on how to take care of by far the most important cause.
We mentioned before that multiple stressors can add together to exceed a threshold and start sensitisation. What can happen is you have a constant source of stress such as pain or emotional stress, but this is not enough to cause sensitisation. If you get another stress on top of this, such as a medical condition or sudden emotional trauma this can push stress levels over the limit. This extra stress can be described as a “fibromyalgia trigger”. If the trigger is removed quite often the original source of stress is enough to maintain the sensitisation. This means the original source must be taken care of as well to stop the fibromyalgia.
Once the nervous system is sensitised the symptoms such as pain itself and the emotional stress caused by not being able to find a solution can further affect the nervous system. This is like when you put a microphone in front of a loud speaker and get a huge squeal. This can make fibromyalgia very difficult to treat. As well as removing the original cause, sometimes some form of temporary symptom relief is needed.
Understanding the real underlying cause of fibromyalgia we can help prevent it. The best way to do this would be to better treat those things that commonly bombard nervous systems.
Better ways of dealing with mental health issues rather than over prescription of drugs.
Dealing with the issues that cause musculoskeletal pain rather than prescribing pain killers and anti-inflammatory drugs.
As you can see the interests of drug companies are the complete opposite to the interests of the people they are supposed to help. They make more money out of providing symptom relieving drugs for these conditions rather than taking care of them properly, and hit the jackpot when your nervous system becomes sensitised. Remember- drug companies control practically all the information your doctor receives.
Our specialty is dealing with the biggest and most inappropriately treated source of this physical pain- (myofascial) trigger points. These are the ones the scientists injected and greatly relieved the fibromyalgia. In the rest of this guide we will discuss why trigger points are such a huge problem and the evidence that treating them helps, or you can go straight to our guide on how to treat them yourself at home.
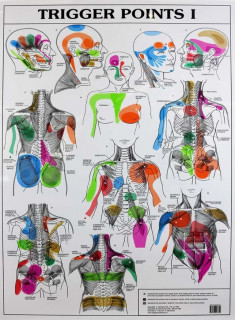
Trigger points are those tender lumps in your muscles that therapists find. They are arguably the biggest cause of musculo-skeletal pain such as back neck and shoulder pain. For more information please see our Complete guide to (myofascial) trigger points. As we will see, because they are so common and generally poorly treated most people have some trigger point pain bombarding their nervous system. Therefore trigger points are generally involved, either as the main cause or providing the “base load” that fibromyalgia triggers add to.
Scientists have done the following research indicating that trigger points were a likely cause.
Finally, they tested this theory by injecting the trigger points with anaesthetic. This stopped the trigger points bombarding the nervous system with pain. The nervous system settled down and the fibromyalgia symptoms were relieved (10)
The reasons trigger points are able to bombard your nervous system with pain for such long periods of time are:
Despite being so common and a massive cause of pain this information usually does not get to doctors. As an example a study of shoulder pain found that trigger points were the major cause and treating them gave excellent results (28). Despite this examples of medical journal articles on how to diagnose and treat shoulder pain make no mention of trigger points (29–31). Instead they are advised prescribe drugs and therapies that do not address the problem.
If trigger points are diagnosed they are too often inadequately treated. As we discuss in our article Why trigger points keep coming back most treatments for trigger points merely temporarily relieve their symptoms but do not eliminate the trigger points. In our guide How to treat trigger points at home we give you an effective home therapy designed to completely eliminate them.
DrGraeme massagers were originally built by Dr Graeme for use in his clinic, and to prescribe to his patients for additional self use at home. Now these are used by colleagues and other professionals for similar purposes. If you are a professional and wish to know more about this therapy, or possibly get a sample massager to trial please check out our practitioner page.
We are continually adding more information on research and uses. Subscribe below to have us email them to you "hot off the press".

Several years ago Dr Graeme, a Chiropractor practicing in Victoria, Australia was looking for a serious hand held massager his patients could use at home to get the extra quality massage they needed. The ones he found in the shops and on-line for home use looked nice but were not serious, and... read more
Fibromyalgia is a sensitisation of the nervous system which causes pain to be amplified plus a host of other symptoms. While there are... Read Article
Massage guns are heavily marketed as a substitute for professional therapists, providing benefits such as sports recovery and pain... Read Article
Many clinical trials have shown that massage reduces anxiety, along with a range of other symptoms such as pain, depression and high... Read Article
Massage is said to help healing and recovery. It certainly does, and in this article I’ll show you scientific evidence of some pretty... Read Article
Treating or releasing trigger points yourself is actually extremely easy. With a bit of instruction and practice you can easily find the... Read Article
Massage and trigger point therapy are widely used to treat back pain. I this article we’ll discuss how these may help with your problem,... Read Article
Cellulite is a very common problem which can be unsightly and have unpleasant symptoms. Common treatments include lasers, needles,... Read Article
Do not refresh or leave this page until loading complete.