An easy safe way to improve sleep quality while reducing anxiety, heart rate and blood pressure
A recent study published in the journal Asian Pacific Journal of Cancer Prevention showed that a simple 15 minute back massage each day... Read Article

(Myofascial) trigger points are arguably the biggest cause of shoulder pain. They cause pain both directly by referring pain, and indirectly by altering the mechanics of the shoulder joint causing impingement syndromes (pinching). Scientists have found that trigger points in 17 different muscles are commonly involved, and that treating these gives excellent relief.
In this article we will discuss what trigger points are, how they cause shoulder pain, and most importantly what you can do about it.
What are trigger points
How trigger points cause shoulder pain
Why shoulder pain keeps coming back
The solution
The treatment of trigger points
Professionals
Appendix: muscles found to directly cause shoulder pain
References
Trigger points are those tender lumps in muscles that massage therapists find. Scientists have found that those lumps are parts of the muscle that have gone into spasm or cramp. As discussed in our article Trigger point basics these create a chain reaction which causes them to “lock on” and continue to grow. They start as small lumps that are only evident when a therapist presses on them, but can continue to develop until they can hurt all the time.
As discussed below trigger points can cause shoulder pain both directly and indirectly.
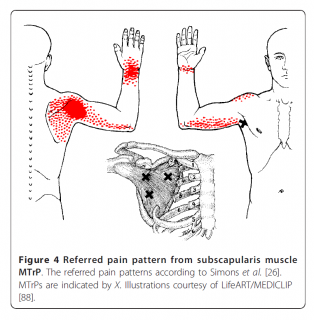
Trigger points can directly cause shoulder pain by referring or "shooting" pain. This diagram shows an example of one muscle that sits under your shoulder blade and can shoot pain to the back of your shoulder and even to your wrist. Scientists have identified trigger points in many muscles that can refer pain to your shoulder. We list these in Appendix one below. One clinical trial confirmed these as a major cause of shoulder pain. When they pressed on the trigger points the pain they produced generally matched the shoulder pain experienced by the patients (3)
For a start trigger points only shoot pain when you press on them. It is not until they are more developed and aggravated that they start shooting pain spontaneously. However, as we'll show in the next section they commonly cause shoulder pain indirectly long before then.
Trigger points indirectly cause shoulder pain by altering the posture and movement of your shoulder joint, creating abnormal stress and possibly pinching. As discussed in our article Trigger point basics trigger points do this by causing muscle to tighten and not be able to work normally. Here we'll show you the basic principles of how this works, then two specific ways this can affect the balance and movement of your shoulder.

A muscle containing a trigger point will be abnormally tight. As this simple diagram shows, when this happens the tension of muscles supporting your spine and joints becomes out of balance.
This becomes futher complicated because those muscles also lose their ability to work normally, so your nervous system needs to change movements and recruit other muscles to compensate.
The end result of these is:
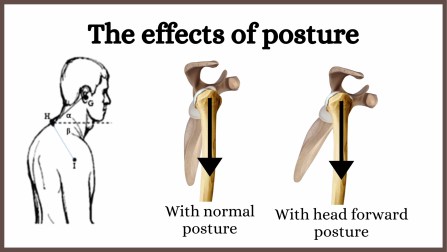
Trigger points in the muscles supporting your trunk, neck and head can cause an imbalance resulting in a head and shoulders forward posture as shown in this diagram. This changes the angle of your shoulder joint, creating abnormal stresses.
As an extra note, there are other causes of posture like this, with one of the most common being issues with the spine.
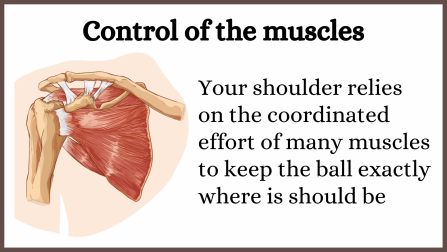
Your shoulder joint has a very large ball like surface sitting in a shallow socket, making it very unstable. To keep the ball sitting exactly where it should be you have a team of muscles as shown in this diagram. If any of those muscles have trigger points they become tight and unable to work normally. The ball will not sit in the socket where it should.
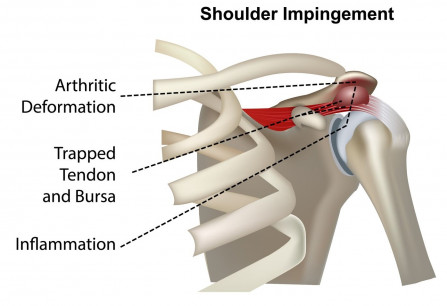
With an abnormal angle and the muscles no longer able to hold the shoulder joint in the right position parts can pinch as the shoulder moves. This is called "impingement syndrome", and is one of the most common medical diagnosis for shoulder pain.
Normally the large ball like part is kept in smooth even contact with the shallow socket. However, without normal control the pressure can become uneven, or only parts of the joint contact. This will cause the joint to wear quickly, eventually resulting in degenerative or arthritic changes seen on x/rays.
To give it to you perfectly straight there are two main reasons shoulder pain either doesn't go away or keeps coming back.
Let's look at each of these.
Despite all the evidence to showing that trigger points cause shoulder pain and the many clinical trials showing that trigger point therapies relieve this pain (1,5–9) trigger points are barely mentioned in medical journals.
Example One:
The article Clinical evaluation of non-arthritic shoulder pain: diagnosis and management (18) in medical journal Physician and Sports Medicine makes no mention of trigger points
Example Two:
The articles Chronic shoulder pain: part I Evaluation and Diagnosis and part II treatment (19,20) in the journal American Family Physician tells doctors that if they do notice a trigger point it is probably fibromyalgia instead.
Because of the heavy influence of drug companies on medical journals it is a common problem that causative issues are ignored and doctors are advised to prescribe symptom relieving drugs.
Shoulder impingement (pinching) is the most common medical diagnosis (10). Doctors recognise that tissues become inflamed, painful and eventually damaged. However, rather than correct the cause of the abnormal function doctors are instructed to prescribe analgesics, anti-inflammatory drugs and cortisone needles, plus of course surgery when the secondary damage gets worse (18,20).
To the uninformed exercises sound like a good idea. However as discussed in our article on functional rehabilitation the abnormal shoulder function is the body's attempt to compensate for parts that are unable to work properly, and as long as the part is abnormal it will keep doing it. That can't be corrected with exercises (25,26). The only way is to restore normal function to the problem part.
The important thing to understand is that if the ball is moving around abnormally in the socket pinching and creating abnormal stresses it's going to do exactly the same thing when doing exercises. This will just cause further long term damage.
If trigger points are diagnosed they generally continue to cause pain because most treatments are merely designed to temporarily stop them shooting pain. This means the trigger points are still there indirectly causing pain, and start shooting pain directly again when re-aggravated.
This applies whether it's a trigger point release seen on YouTube or a course of needles, laser or some other therapy provided by a respected professional. We believe it is:
We is discussed in our article Trigger point treatment: deactivation or elimination, however will show you one piece of evidence to confirm it is all correct,
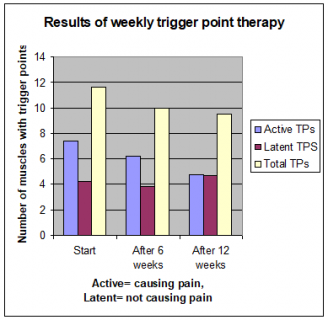
This chart shows that when the best PhD. trigger point researchers used 12 very extensive weekly trigger point sessions the pain was relieved, but 2/3 of the trigger points were still there (10). In those sessions they spent 45 minutes just working on the shoulders, and used a combination of several therapies. If they could do that and only eliminate 1/3 of the trigger points a hand full of sessions with just one therapy is hardly going to make a dent in the trigger point numbers.
The trial above shows that a typical course of say six sessions of dry needles or laser will just be very expensive temporary pain relief. However, it does point the way to a better solution. Those 12 extensive sessions did manage to relieve much of the shoulder pain and eliminate 1/3 of the trigger points. This suggests that if the therapy is continued further trigger points will be eliminated. Of course you will need an effective home therapy so you can do at least some yourself otherwise it will become very expensive.
This forms the basis of our shoulder pain solution. Full details are in our article Massage and trigger point therapy for shoulder pain: with self care options. This is a step by step guide which includes:
Upper trapezius muscle
Middle trapezius muscle
Lower trapezius muscle
Infraspinatus muscle
Supraspinatus muscle
Subscapularis muscle
Teres minor muscle
Teres major muscle
Anterior deltoid muscle
Middle deltoid muscle
Posterior deltoid muscle
Pectoralis major muscle
Pectoralis minor muscle
Biceps brachii muscle
Triceps brachii muscle
We are continually adding more information on research and uses. Subscribe below to have us email them to you "hot off the press".

Several years ago Dr Graeme, a Chiropractor practicing in Victoria, Australia was looking for a serious hand held massager his patients could use at home to get the extra quality massage they needed. The ones he found in the shops and on-line for home use looked nice but were not serious, and... read more
A recent study published in the journal Asian Pacific Journal of Cancer Prevention showed that a simple 15 minute back massage each day... Read Article
Most movements require the co-ordinated contraction and relaxation of numerous muscles. The neurological control of this is known as a... Read Article
Trigger points are those tender lumps in muscles that therapists find. This article covers what they are, what they do, and how they are... Read Article
Tennis elbow is a painful and disabling condition that is said to develop through overuse, but why does it then refuse to heal and defy... Read Article
When we look at the root cause of fibromyalgia we need to look at two levels: 1. the malfunction of the nervous system which causes the... Read Article
As a chiropractor for over 27 years vertebral subluxation complexes are a very real problem that can cause pain, long term spinal damage... Read Article
Most professional athletes and sports clubs make heavy use of massage type treatments. The ability to do self massage using a hand held... Read Article
In this article we will discuss the health and wellness benefits of regular or wellness massages that have been scientifically... Read Article
Do not refresh or leave this page until loading complete.